Geschreven door Eline Te Braake en Christiane Grünloh
RE-SAMPLE is een Europees project dat zich richt op mensen met COPD en andere chronische aandoeningen. Het doel van RE-SAMPLE is om een technologie te ontwikkelen die patiënten en hun zorgverleners ondersteunt. Deze technologie zal patiënten helpen hun COPD en andere chronische aandoeningen te beheren. Samen met 9 andere partners werkt RRD samen aan dit project om de RE-SAMPLE technologie vorm te geven en te ontwikkelen. Het project is gestart in maart 2021 en zal in totaal 4 jaar duren. RE-SAMPLE heeft financiering ontvangen van Horizon (Grant agreement No. 965315).
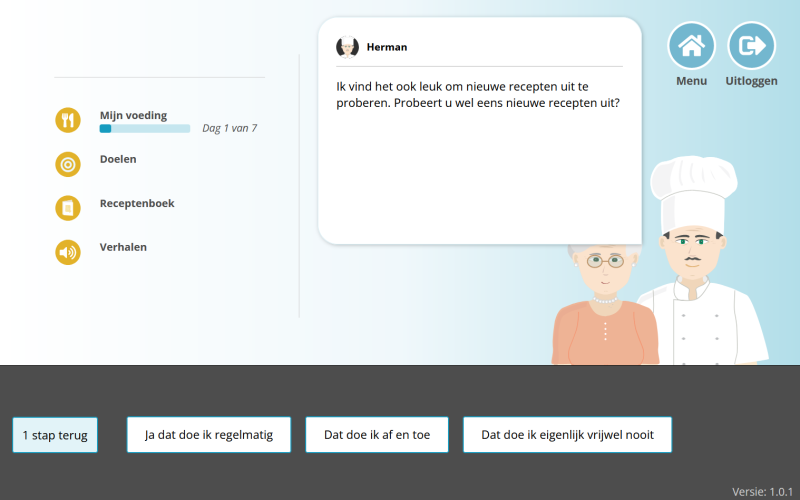
GEBRUIKERSGERICHT. Bij het ontwerpen van een eHealth interventie is het belangrijk om rekening te houden met de behoeften en wensen van degenen die er gebruik van gaan maken. Uiteindelijk willen we dat RE-SAMPLE een meerwaarde heeft in de praktijk voor zowel mensen met COPD als hun zorgprofessionals. We willen natuurlijk ook dat na het project, RE-SAMPLE daadwerkelijk succesvol geïmplementeerd wordt in de gezondheidszorg. Om dit te doen, moeten we leren van de houdingen, ervaringen, en behoeftes van mensen met COPD en hun zorgverleners. Omdat zij allemaal experts in het veld zijn, weten zij het beste wat er momenteel ontbreekt of wat er juist al heel goed gaat. Deze informatie kan ons helpen bij het ontwikkelen van een technologie die daadwerkelijk nuttig voor hen is.
Sinds de start van RE-SAMPLE hebben we al heel wat verschillende onderzoeken uitgevoerd. We hadden de kans om met veel mensen met COPD en zorgverleners te praten om zo meer te weten te komen over COPD, de ervaringen met leven en omgaan met COPD, en voorkeuren met betrekking tot COPD-management. Dit leverde veel nuttige informatie op. Deze input heeft ons erg geholpen bij het vormgeven van de RE-SAMPLE technologie. Om u een idee te geven van wat we tot nu toe hebben ontdekt, heeft RRD een samenvattende video gemaakt met enkele hoogtepunten.
U kunt deze video hieronder bekijken!
Hoewel er al veel informatie wordt verzameld, hebben we in de toekomst ook steeds input nodig van zowel zorgverleners als mensen met COPD! Wilt u na het horen van RE-SAMPLE ook met ons meedenken en ons feedback geven?
Neem dan gerust contact met ons op!
Dit kunt u doen door een e-mail te sturen naar Christiane Grünloh (c.grunloh@rrd.nl) of Eline te Braake (e.tebraake@rrd.nl)