Written by: Marian Hurmuz
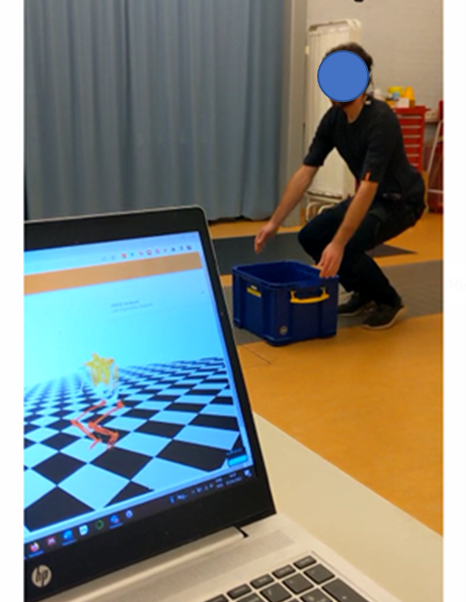
Data-driven intent recognition using electromyography (EMG) has the potential to make actuated prosthesis more intuitive. Although electromyography has its challenges, it also forms an opportunity to realize more intuitive control of prostheses through intent recognition. Robert Schulte aimed to investigate data-driven intent recognition strategies in the lower-limb using EMG. Last week Thursday (8th of December, 2022), Robert defended his PhD thesis, which you can find here Finding.
His thesis covers the following topics:
- Developing and validating a synchronisation method for wearable motion capture and EMG measurement systems.
- Collecting a large database of kinematic and EMG data, MyPredict, containing 55 participants measured in 85 measurement moments.
- Investigating the use of genetic algorithms to construct optimised feature sets to be used in lower limb prosthetic control.
- Investigating whether concept drift is an issue in lower limb pattern recognition.
- Comparing three adaptation approaches to circumvent the concept drift: entropy-based, based on backward prediction, and a combination of the two.
- Comparing three modelling frameworks to estimate knee torque in non-weight-bearing situations: convolutional neural network (CNN), neuromusculoskeletal model (NMS), and a hybrid model of both.
Robert ends his thesis by concluding that data-driven intent recognition has the potential to make prostheses more intuitive, thereby possibly leading to better prosthesis control.
We are very proud of Robert and his hard work at RRD! With ending his PhD, there is no end to working with data. Robert started working at Datavibes in Gouda as a Data Engineer/Data Scientist. He continues working with data, but now in a less scientific environment. We wish him the best of luck in his future career!